News & Insights
Securing off-grid power: the role of microgrids in resilient hospitals
Microgrids are an innovative solution to empower healthcare facilities with sustainable, on-site power generation and distribution. This article delves into the multifaceted advantages of implementing microgrids for full operations, from enhancing operational continuity to minimizing long-term costs and environmental impact.

Hospitals are reevaluating their power strategies amid an unpredictable energy environment. Regulations require a primary power source, usually the utility grid, with emergency generators as backup. However, relying solely on this setup poses challenges. Backup generators offer limited support, dependent on fuel supply, and grid disruptions force hospitals to limit operations to critical care only. This impacts patient services and strains hospital resources, highlighting the need for a more resilient power solution.
A more holistic and sustainable approach to this challenge is the integration of microgrids. These advanced systems signify a paradigm shift in how hospitals manage power. Microgrids offer a self-sufficient power solution, capable of operating independently from the traditional grid. Hospitals can maintain full operational capacity without being vulnerable to external power disruptions, ensuring uninterrupted patient care and smoother hospital operations.
Microgrid technology overview
One of the most significant advantages of microgrids is their ability to operate either connected to a power grid or independently in “island mode” and generate their own power. Here are the key components to a microgrid:
- Energy generation sources: Microgrids utilize a diverse mix of energy sources. This can include renewable sources such as solar panels or wind turbines, solutions like solid oxide fuel cells, and more traditional sources like diesel generators and natural gas. The mix is tailored to ensure reliability and sustainability in the context of the area served.
- Distribution infrastructure: This refers to the network of wires, switches, and other equipment that distributes electricity within the microgrid. It’s designed to be robust and flexible, capable of adjusting to changing power demands and sources.
- Control systems: These sophisticated systems are the brains of the microgrid. They monitor and manage energy production, storage, and distribution, ensuring efficient and stable operation. This includes balancing supply and demand and switching between grid-connected and island modes.
- Grid interconnection: Microgrids are usually connected to the main utility grid. This connection allows them to draw additional power when needed and, conversely, supply excess power back to the main grid. The ability to disconnect and operate independently creates resilience during main grid outages.
- Battery storage systems (BESS): Battery storage systems are an option for a microgrid system to store the excess energy generated. This stored energy can be used for maintaining power supplies during periods of high demand or when renewable sources aren’t generating power (such as at night or on cloudy days).
How microgrids operate to serve hospital power needs
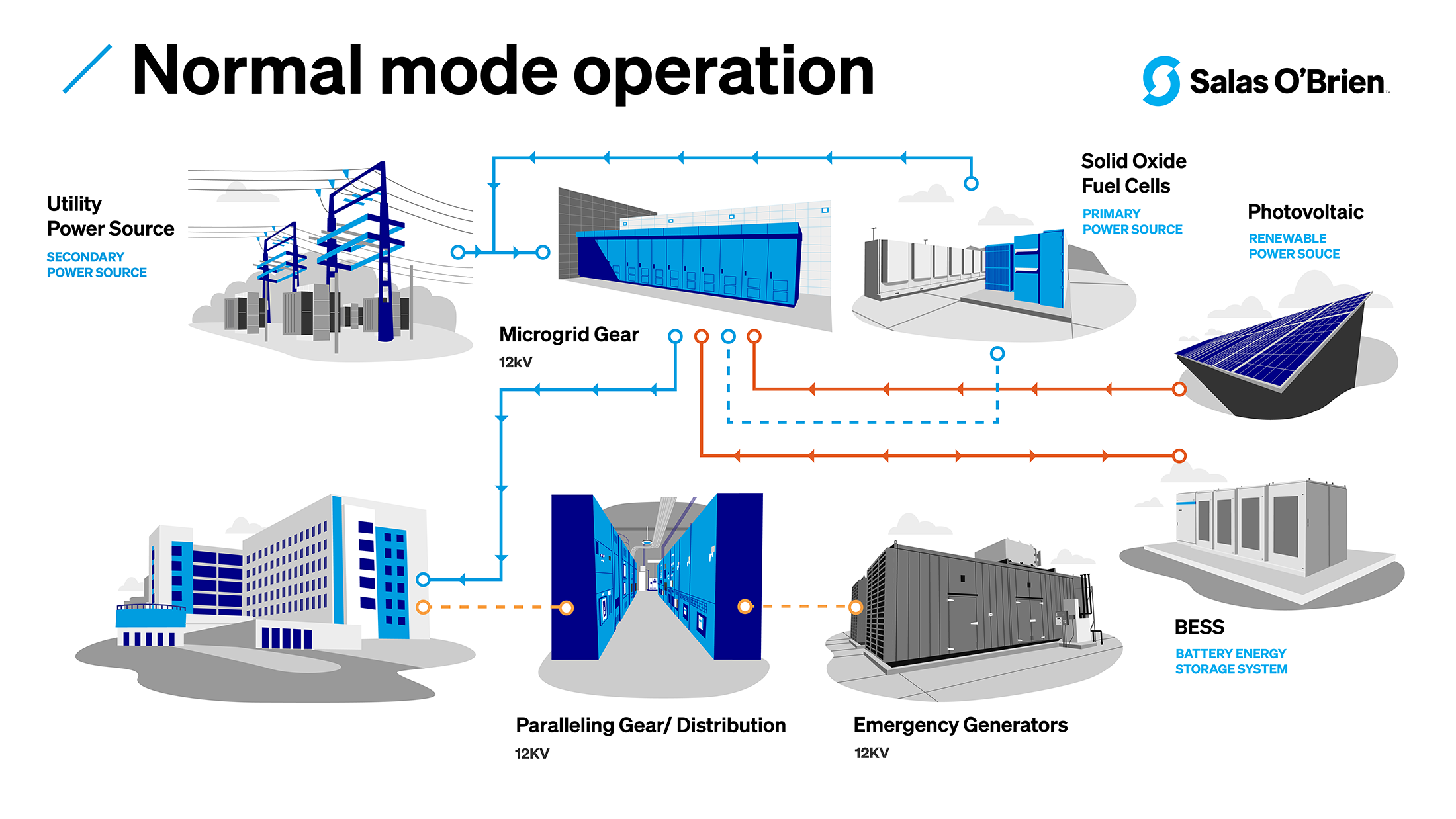
In normal operation, the hospital utilizes onsite power as primary source and utility grid as secondary source.
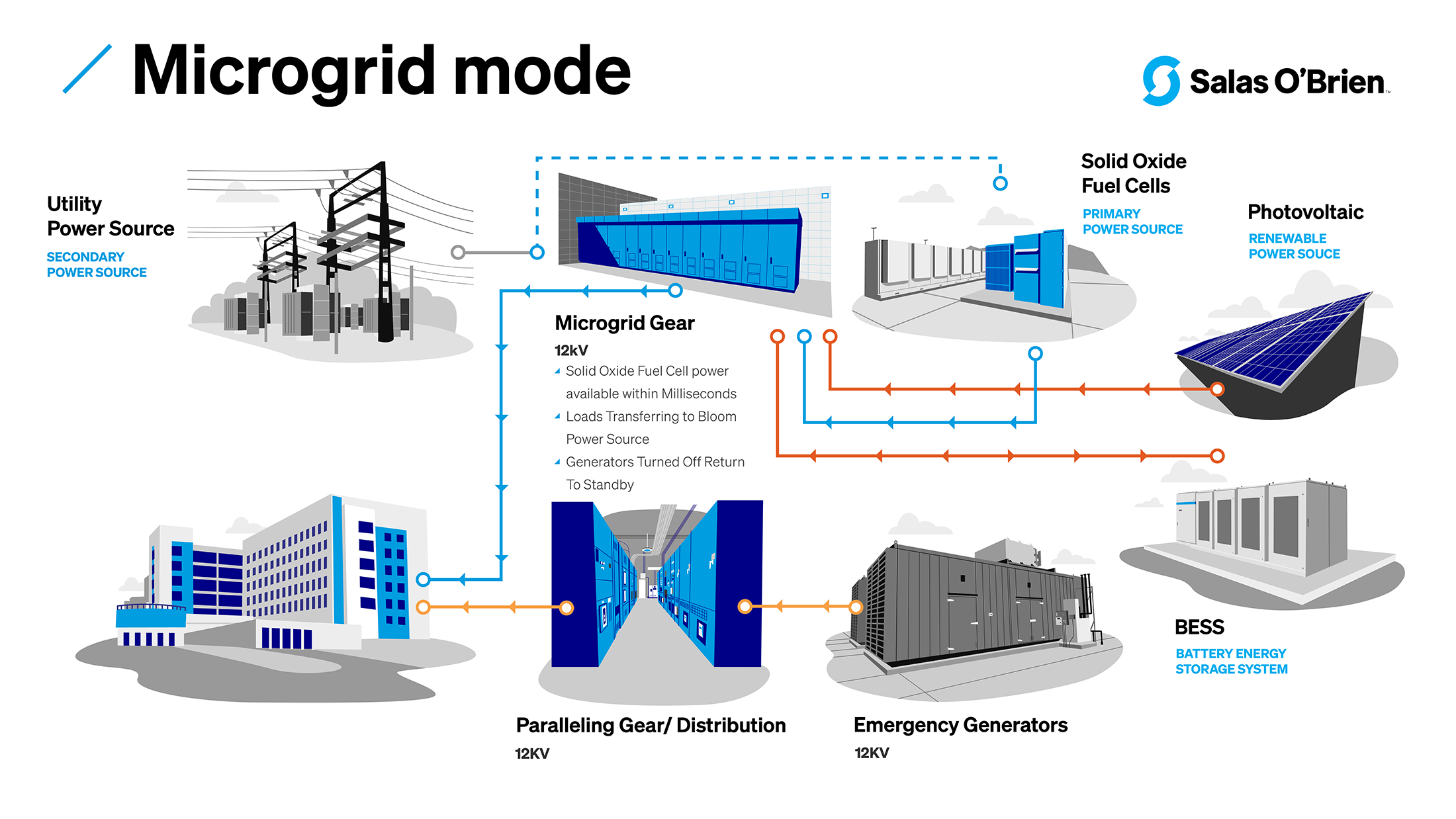
In microgrid mode, power is produced by the energy generating sources (like solid oxide fuel cells, PV, and BESS) providing power to the hospital with both emergency generators and the utility grid providing power backup.
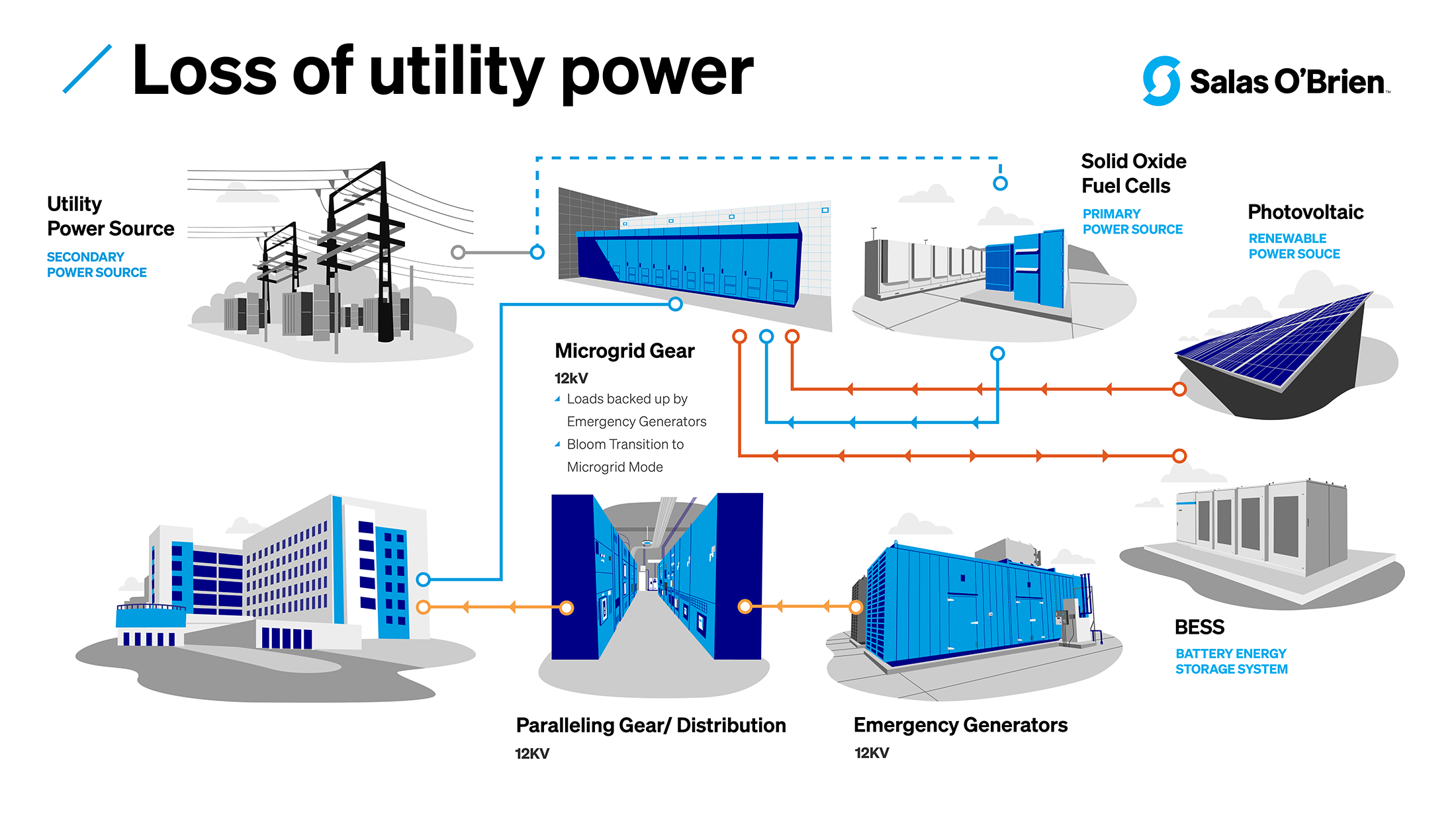
With a loss of utility power, the hospital has access to power from a source—such as solid oxide fuel cells, PV, and BESS—with backup from emergency generators.
Benefits of microgrids for hospitals
Salas O’Brien is working with many hospitals to implement microgrids in their energy planning. Here are some key advantages we see for clients in healthcare systems:
- Maintaining continuous operations: Microgrids can provide an extra layer of protection to the power supply, which is crucial for hospitals which operate 24/7. In the event of a grid outage, a microgrid can disconnect from the main grid and continue to power the hospital independently. This feature protects patient care and alleviates the challenges presented by rescheduling surgeries.
- Cost savings: Although there’s an initial investment, microgrids can lead to significant cost savings in the long run. By generating power on site, hospitals can reduce their energy bills, especially during peak demand times when energy prices are highest. Additionally, hospitals can potentially generate revenue by selling energy back to the grid through programs like demand response.
- Reduction in carbon footprint: As healthcare facilities aim to become more sustainable, microgrids offer a way to decrease carbon emissions. By integrating renewable energy sources, hospitals can significantly reduce their environmental impact.
- Scalability and flexibility: Microgrids can be designed to be scalable and flexible, allowing hospitals to expand or modify their energy systems as their needs change. This adaptability supports hospitals that may need to grow or adjust their facilities over time.
- Regulatory compliance: Hospitals often face stringent regulatory requirements regarding emergency power and backup systems. Microgrids can help hospitals meet these requirements more effectively than traditional backup generators.
- Predictive maintenance: Modern microgrids often come equipped with advanced, ongoing monitoring systems. These systems can predict and alert staff to maintenance needs, ensuring that power systems are operating optimally and reducing the risk of unexpected failures.
In addition to the practical advantages for hospital operations, there is also a public advantage: in times of widespread power outages, hospitals with microgrids can serve as safe havens for the community by providing critical services not only for patients but also for local residents in need.
What hospital administrators and facility planners need to know about microgrids for hospitals
Microgrids represent a forward-thinking approach to energy management, particularly for expansive sites like hospitals. However, a significant challenge in implementing these systems is the lag in building codes and regulatory standards. This misalignment can necessitate modifications or variances in project plans, introducing added complexity and potential delays.
For microgrids to be most effective, they must be designed with the entire site in mind and consider both current needs and future expansions. While numerous vendors offer solutions, success hinges on developing a comprehensive, well-engineered power plan. This plan should seamlessly integrate all elements and encompass not just implementation but also ongoing maintenance.
This holistic energy planning benefits from the guidance of an experienced partner who not only comprehends the end goals but also has a deep understanding of the existing field infrastructure.
Salas O’Brien has a proven track record in assisting hospitals with innovative, resilient, and dependable energy solutions that also prioritize reducing carbon emissions. To explore how a microgrid could advance your energy objectives, connect with us.
For media inquiries on this article, reach out to Stacy Lake, Director of Corporate Communications.

Duc Bui, PE
Duc Bui is an expert in the electrification of healthcare facilities. A leading provider of electrical engineering solutions and an innovator in using low voltage DC power for LED lighting , he holds a US Patent on Direct Current Power Delivery System. Duc specializes in healthcare facilities and pharmaceutical facilities with a strong presence in California serving large corporations such as Kaiser Permanente, Abbott Vascular, Tenet, University of California Irvine, and the University of Southern California. Duc serves as a Principal for Salas O’Brien. Contact him at [email protected].

James McCollum, LEED Green Assoc.
James McCollum specializes in construction and engineering for healthcare. He spent the early part of his career in healthcare construction, then transitioned to serve Kaiser Permanente by becoming Director of Facility Services, a position where he skillfully managed plant operations and physical security. He transitioned into consulting engineering and joined DPB in 2012, which merged in 2022 with Salas O’Brien, a leading multidisciplinary engineering firm. Jim serves as a Principal at Salas O’Brien. Contact him at [email protected].


